如果Osimertinib 奥希替尼(Tagrisso,泰瑞沙)耐药了,接下来到底该怎么办?
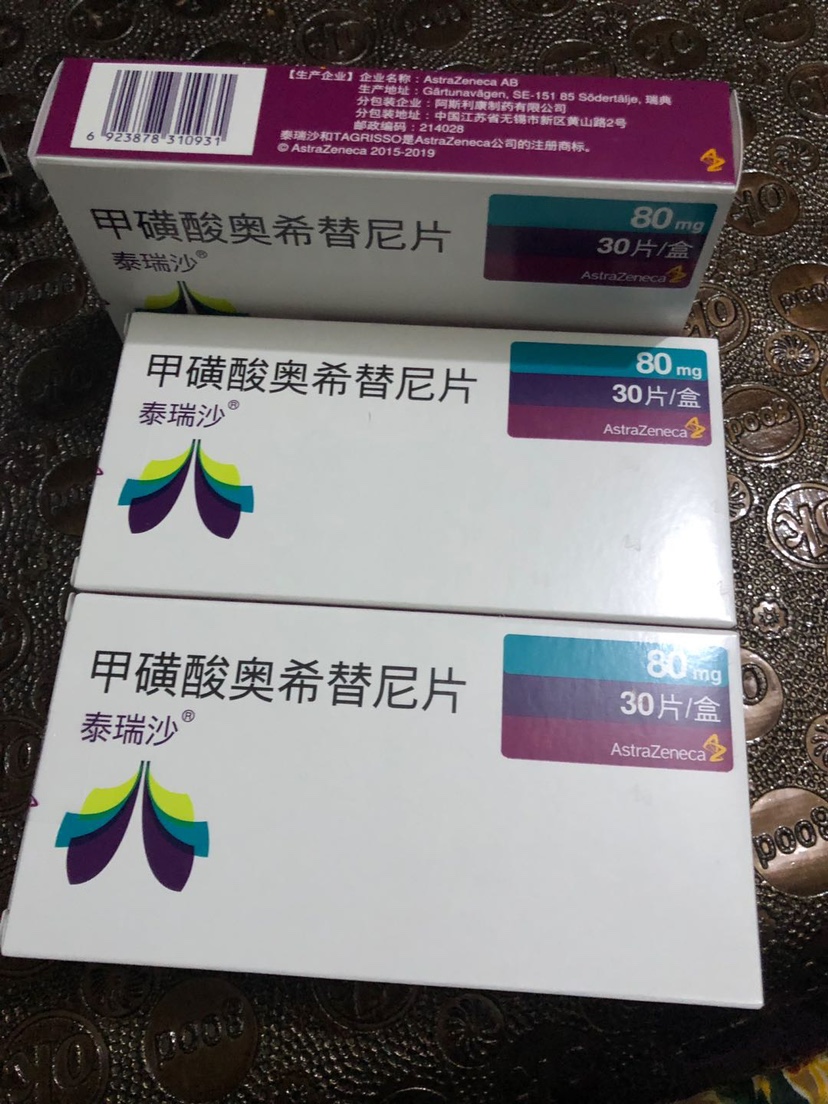
据印度代购了解,随着第三代EGFR靶向药,泰瑞沙在国内上市并正式投入临床使用,一个迫切的问题开始不断萦绕在医学界和病友心头:如果泰瑞沙耐药了,接下来到底该怎么办?首先要搞清楚耐药的原因,携带EGFR T790M突变的晚期肺腺癌患者,接受泰瑞沙等第三代靶向药治疗,中位无疾病进展生存时间约为10-12个月——1年左右,药物耐药以后,上策是尽可能明确耐药的原因。目前来看,耐药的机制主要分为3大类:EGFR基因上又产生的新的突变,其他基因发生了变异,转化为小细胞肺癌。
According to Daigou India, as the third generation egFR-targeting drug Tiresa has been launched in China and officially put into clinical use, an urgent question has been lingering in the medical community and patients' minds: if Tiresa is resistant, what should we do next? First of all, it is necessary to figure out the cause of drug resistance. Patients with advanced lung adenocarcinoma carrying EGFR T790M mutation and receiving tiresa and other third-generation targeted drugs have a median progression-free survival time of about 10-12 months -- about one year. After drug resistance, it is best to identify the cause of drug resistance as much as possible. At present, the mechanisms of drug resistance can be divided into three categories: new mutations in EGFR gene and mutations in other genes, which are transformed into small-cell lung cancer.
据印度代购了解,最常见的是C797S突变,大约占15%-40%的病人是由于产生了这个新的耐药突变,导致了泰瑞沙的失灵,目前针对这个新突变正在研发第4代靶向药。其他的少见耐药突变包括:L718Q,G796D等——解决这类问题的根本途径,就是期待更新的靶向药,能特异性地靶向这类突变,所谓“升级打怪”,以至于无穷罢了。
据印度代购了解,EGFR信号通路被泰瑞沙给阻断了,为了活命,癌细胞可以变着法子激活其他的信号通路,比如HER2扩增,BRAF基因突变,MET基因扩增,KRAS突变等——解决这类问题,或许需要靠同时使用泰瑞沙以及针对性的第二种、第三种靶向药。比如同时携带EGFR和BRAF基因突变的病友,或许可以试一试联合使用泰瑞沙以及BRAF抑制剂。
据印度代购了解,大家都知道肺癌分为两大类——小细胞肺癌和非小细胞肺癌。携带EGFR基因突变的非小细胞肺癌,接受靶向治疗后,一部分会转变为小细胞肺癌,这个现象在接受第一代靶向药的患者中其实不少见,现在也已经报道出现在了小部分服用泰瑞沙的病人身上——对于这类病友,可以考虑联合泰瑞沙和适用于小细胞肺癌的化疗(顺铂+VP-16),可能有效果。
据印度代购了解,除了耐药的原因不同之外,耐药的表现形式也不同;每一种不同模式的疾病进展,应对的策略也不同。缓慢进展:这类病友,全身的一个或多个病灶很缓慢地进展。几厘米的肿瘤,大半年了才增长零点几个厘米。如果是这种情况,继续泰瑞沙治疗,或者泰瑞沙联合一个温和的、单药的化疗,都是可取的。局部进展:病人在接受泰瑞沙治疗过程中,出现某个局部的单发或者少数几个病灶的进展。比如新出现了一个骨转移,或者出现了一个不算大的肝转移。那么可以考虑继续泰瑞沙治疗,同时对进展的局部加一点干预(骨转移可以放疗,肝转移可以介入等)。全面进展:病人出现了全身的、多发的、快速的进展。这类疾病进展是最凶险、预后最差的。一般我们会建议停用泰瑞沙,考虑化疗或者根据耐药的原因,给予针对性的治疗。
According to daigou India, in addition to different reasons for drug resistance, the forms of drug resistance are also different; For each of these different patterns of disease progression, there are different strategies to deal with them. Slow progression: In this group, one or more lesions throughout the body progress very slowly. A tumor of a few centimeters has grown by a few tenths of a centimeter over the past six months. If this is the case, continued tyresa therapy, or tyresa in combination with a mild, monotherapy chemotherapy, may be desirable. Local progression: progression of a single or small number of lesions in a particular area during terisat therapy. For example, there is a new bone metastasis, or there is a small liver metastasis. Therefore, it may be considered to continue tyresa therapy, and at the same time, local intervention (radiotherapy for bone metastases, intervention for liver metastases, etc.) can be added. Overall progress: The patient developed systemic, multiple, and rapid progress. This type of disease progression is the most dangerous and has the worst prognosis. In general, we recommend discontinuing tyresa, considering chemotherapy or, depending on the cause of resistance, targeted treatment.





 咨询客服
咨询客服